English again below
Bildquelle/Image source: BUPA
Die Schnellfassung
Wenn Sie einen pränatalen, konnatalen oder kongenitalen AV-Block °III, einen atrioventrikulärer Block, 3. Grades oder einen kongenitalen kompletten Herzblock ohne sonstige Auffälligkeiten diagnostizieren oder diagnostiziert bekommen, sollten Sie sofort einen Bluttest der Mutter beauftragen um Ro und La AK zu bestimmen! Zusätzlich kann und sollte Anti Phospholipid AK abgenommen werden (Anti Cardiolipin).
Liegt der Herzschlag unter 60 SpM (Schläge pro Minute), ist zudem auf Perikarderguss, Hydrops und (selten) Endokardfibroelastose zu kontrollieren. Ist dieser Befund positiv (also so etwas vorhanden), oder gibt es sonstige Auffälligkeiten, kontaktiert der behandelnde Arzt sofort das nächstgelegene Kinderherzzentrum. Abhängig von der genauen Diagnose ist eine Notfalleinweisung (ggf. mit Rettungswagen) wahrscheinlich! Das Kind ist in akuter Lebensgefahr, eine Schädigung von Organen oder pränataler Entwicklung nicht auszuschließen.
Liegt der Herzschlag unter 60 SpM es liegt aber kein Befund der o.g. Komplikationen oder andere Auffälligkeiten vor, sollte ebenfalls unverzüglich das nächste Kinderherzzentrum kontaktiert werden. Eine sofortige Einweisung ist hier ebenfalls notwendig, in diesem Fall wird möglicherweise noch vor der Einweisung durch Ihren behandelnden Arzt medikamentös der Herzschlag stimuliert (ca. 5-10 Schläge).
Liegt der Herzschlag über 60 SpM und es liegt keine der o.g. Komplikationen vor sind die Chancen recht gut, die negative Entwicklung zu stoppen und abgesehen vom notwendigen Herzschrittmacher ein gesundes Kind zu bekommen. Nein, es ist nicht sicher! Arzt oder Mutter soll sich ebenfalls auf dem schnellsten Weg mit dem nächstgelegenen Kinderherzzentrum in Verbindung setzen und zeitnah einen Termin vereinbaren! Zeitnah bedeutet, dass dies nicht am selben Tag sein muss! Wichtig ist es, ein Kinderherzzentrum einzubinden, nicht jedes Pränatalzentrum und nicht jeder Arzt hat hier die notwendige Erfahrung!
Mehr Informationen zur weiteren Behandlung folgend. Nun aber erstmal zur Diagnose…
Was ist eigentlich ein pränataler AV-Block 3. Grades?
Zuerst einmal wird der unterschiedlich beschrieben, mal als pränatal (vorgeburtlich), mal als kongenital oder konnatal (beides für “angeboren”), mal als AV-Block 3. Grades, mal mit einer Bradykardie (verlangsamter Herzschlag) in Zusammenhang gebraucht, mal vollständig als atrioventrikulärer Block oder auch eher umgangssprachlich als vollständiger oder kompletter Herzblock bezeichnet, mal als AVB oder AVB3 abgekürzt.
Wer diese Diagnose das erste Mal hört, weiss damit nichts anzufangen und wird im Internet mit vielen Fehlinformationen versorgt, die meisten davon panikerzeugend. Wie wir erfahren haben geht dies auch erfahrenen Ärzten so, ist diese Diagnose doch sehr, sehr selten – nur etwa eine aus 20.000 Lebendgeburten! Bei über 660.000 Geburten 2012 wären dies 33 Geburten / Jahr in Deutschland, an der MH Hannover sind dies wohl 1-2 Fälle im Jahr.
Ohne die Diagnose verharmlosen zu wollen: Wenn Sie sich damit konfrontiert sehen, ist etwas schlimmes passiert. Wahrscheinlich wurden die Muskelstränge des Reizleitungssystems1, die den Herzschlag steuern am Herzen Ihres Kindes irreparabel geschädigt.
So schlimm diese Diagnose an sich auch ist, alles weitere kann gehandhabt werden! Und wenn alles gut läuft, bekommt Ihr Kind “lediglich” einen Herzschrittmacher, aber diese bedeuten in der Realität nur geringe Einschränkungen! Bitte lesen Sie weiter!
![]() Die folgenden Informationen sind derzeit nicht wissenschaftlich fundiert sondern beruhen auf medizinischen Erfahrungen, Einschätzungen und Empfehlungen. Aufgrund der Seltenheit der Diagnose gibt es nach unserem Wissen derzeit keine belastbaren2 Studien und Ergebnisse!
Die folgenden Informationen sind derzeit nicht wissenschaftlich fundiert sondern beruhen auf medizinischen Erfahrungen, Einschätzungen und Empfehlungen. Aufgrund der Seltenheit der Diagnose gibt es nach unserem Wissen derzeit keine belastbaren2 Studien und Ergebnisse!
Es gibt diverse Studien an kleineren Gruppen, aufgrund derer bestimmte Behandlungsmöglichkeiten als vielversprechend angesehen werden. Diese Studien finden Sie am Ende der Seite unter weitere Lektüre.
Die wahrscheinlichen Gründe für einen pränatalen AV-Block 3. Grades
Die Diagnose eines pränatalen AV-Block 3. Grades (vollständig) gibt es ein drei Ausprägungen, die jeweils ein Drittel der Fälle betreffen.
Variante 1 ist im Zusammenhang mit einem sogenannten kongenitalen, also angeborenen Herzfehler, wobei hier generell das Herz und die organische Entwicklung mit betroffen sind.
Variante 2 wird als idiophatisch bezeichnet, d.h. es gibt keinen nachvollziehbaren Grund.
Variante 3 ist im Zusammenhang mit einer “negativen” Autoimmunreaktion der Mutter. Von einer “Erkrankung” ist hier nicht unbedingt zu sprechen, da Autoimmunreaktionen, die Bildung von Antikörpern “tendenziell gesund” sind. Richten diese sich jedoch gegen gesundes, körpereigenes Gewebe, machen sie krank und es wird wie auch hier von einer Autoimmunerkrankung gesprochen.
Generell ist dies meines Wissens die einzige bisher bestätigte Ursache, die wir hier entsprechend versuchen können verständlich zu machen.
AV-Block 3. Grades + Sjögren Syndrom
Diese Ursache des AV-Block ist wohl eine rheumatische Reaktion, ein sogenanntes Sjögren Syndrom bei der Mutter, die lange vor der Schwangerschaft passiert sein kann. Oft wird diese Erkrankung nicht einmal bemerkt! Durch diese rheumatische Reaktion hat der Körper aber Antikörper entwickelt, sogenannte Ro und La AK. die sich dann unbemerkt im Körper aufhalten.
Diese Antikörper wurden durch die Immunabwehr der Mutter gebildet um die eigene “Erkrankung” zu bekämpfen, sind daher nicht etwa bösartig.
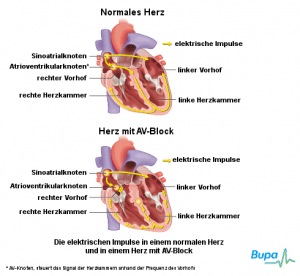
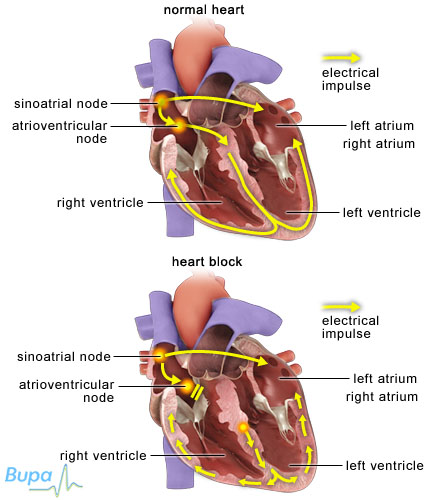
Nun kommt es zur Schwangerschaft. Zwischen der 18. und 20. Schwangerschaftswoche wandern Antikörper, darunter auch eben die Ro und La AK durch die Plazenta in den Körper des Kindes. An sich ja eine gute Idee, auf diese Weise bekommt das Kind nun die Immunisierung der Mutter. Im Falle der Ro und La AK Antikörper kommt es nun aber zu einer Fehlreaktion. Diese Antikörper “verstehen” die sich entwickelnden Reizleiterbahnen1, die die Signale zum Herzschlag am Herzen des Kindes transportieren als rheumatisch. Bei der entsprechenden Reaktion zerstören diese nun diese sich entwickelnden Reizleiterbahnen1! Dies betrifft vor allem die Verbindung vom Nervenknoten1 am Herz, dem sogenannten AV-Knoten, zu den Hauptkammern, daher der Name der Diagnose. Es gibt hier unterschiedliche Ausprägungen, von einer teilweisen Störung bis hin zur kompletten Zerstörung, die man dann als 3. Grades (auch III geschrieben) bezeichnet.
In vielen Fällen ist dies für das Kind tödlich. Aber dann würden Sie dies hier nicht lesen. In den anderen Fällen wird das Herz aufgrund sekundärer Reize und Nervenverbindungen weiter zum Schlagen angeregt, allerdings deutlich verlangsamt. Ob ein Zusammenhang zwischen mütterlichem Herzschlag und dem verbliebenen Herzschlag besteht habe ich widersprüchliche Informationen.
Im mir bekannten, eigenen Fall brach der Herzschlag auf 62-63 Schläge pro Minute (SpM) ein. Normal wären 110-160 SpM.
Ich wurde gebeten, hier auch den noch seltener auftretenden systemischen Lupus erythematodes anzugeben (auch Lupus oder SLE genannt). Sjörgen-Syndron und systemischer Lupus Erythemathodes sind zwei Ausprägungen einer rheumatischen Autoimmunerkrankung mit unterschiedlichen Symptomen, diese sollten beide mit der Prüfung auf Ro und LaAK Antikörper erkannt werden.
Die Diagnose. Und nun?
 Wichtig ist: Schnelligkeit! Da die Antikörper ja auch im Kind noch aktiv sind, sind weitere Schädigungen nicht auszuschließen, eher wohl sogar wahrscheinlich. Daher muss schnellstens gehandelt werden. Nicht um die Situation zu verbessern, sondern um weitere Schäden und Schädigungen zu verhindern.
Wichtig ist: Schnelligkeit! Da die Antikörper ja auch im Kind noch aktiv sind, sind weitere Schädigungen nicht auszuschließen, eher wohl sogar wahrscheinlich. Daher muss schnellstens gehandelt werden. Nicht um die Situation zu verbessern, sondern um weitere Schäden und Schädigungen zu verhindern.
Diese Diagnose allein besagt nichts, aber auch gar nichts über die weiteren Überlebenschancen des Kindes. Auch ist diese Diagnose kein Anzeichen für irgendeine sonstige “Behinderung” des Kindes!
Wichtig ist vor allem, weitere Komplikationen auszuschließen, sowie die weitere Schädigung zu verhindern.
Als Komplikationen sind vor allem die bereits oben erwähnten Perikarderguss, Hydrops und Endokardfibroelastose zu betrachten (die Links öffnen ein neues Fenster). Wobei ein kleiner Perikarderguss wohl relativ “normal” ist und bspw. nur beobachtet wird. Dies können die Fachärzte des Kinderherzzentrums besser beurteilen!
Die Verhinderung weiterer Schädigungen der Entwicklung von Reizleitern1 des Kindes ist etwas schwierig. Bei der Seltenheit der Erkrankung gibt es verständlicherweise keine prospektiven2 Studien. Aufbauend auf früheren, dortigen Untersuchungen gilt am Hospital for Sick Children in Toronto (Canada) die Therapierichtlinie, dass den Müttern bei der fetalen Diagnose eines kompletten AV-Block mit einer fetalen Herzfrequenz unter 55 SpM Dexamethason und ein Betamimetikum (zur Stimulierung der ß-Rezeptoren, sozusagen das Gegenteil eines ß-Blockers) gegeben wird. Dem widerspricht andererseits die “große AEPC-Studie” (Link zu englischer Veröffentlichung), die keine Verbesserung der Überlebensrate der Kinder unter Kortison-Gabe fand. Hier erwiesen sich ein Diagnosezeitpunkt unter 20 Wochen, eine Herzfrequenz unter 50/min, ein Hydrops und eine eingeschränkte LV-Funktion als prognostisch besonders ungünstig. Andererseits wird von anderen Autoren (wie auch Prof. Dr. von Kaisenberg an der Medizinischen Hochschule Hannover) eine Steroid-Behandlung zur Vermeidung eines Hydrops empfohlen.
Diese hat aber auch (wie aber jede Behandlung) Nebenwirkungen. Die wichtigste Nebenwirkung ist eine Veränderung des organischen Gewebes des Gehirns. Es gibt aber nach derzeitigem medizinischen Stand abgesehen von dieser Veränderung des Gewebes keine negativen Begleiterscheinungen. Es gibt aber eben auch keine verlässlichen Informationen, die solche negativen Nebenwirkungen ausschließen.
Was sich in den bisherigen Versuchen gezeigt hat, ist, dass diese Behandlung die Gefahr weiterer Schädigungen weitgehend reduziert, die Überlebenschance der behandelten Kinder stieg dabei von 80% vor Einführung der Behandlung auf 95% danach. Vorher lag die Überlebenschance des Kindes für das erste Jahr nach der Geburt bei 47%. Obwohl es keine harten Zahlen gibt, kann man folgende Interpretation als wahrscheinlich ansehen:
“Obwohl prospektive Studien fehlen, werden fluoride Corticoide bei Feten mit inkompletter AV-Blockierung und Hydrops empfohlen, Ist der AV-Block erst komplett etabliert, so ist keine Regression, eher ein Fortschreiten der Blockierung von zweit- zu drittgradigen Blockierungen beschrieben worden.” (Quelle). Aber auch beim AV-Block 3. Grades besteht die Gefahr weiterer Schädigungen durch die Antikörper! Daher ist eine entsprechende Behandlung bis Ende der Schwangerschaft wohl sinnvoll!
Es geht bei der Behandlung darum, das Kind möglichst lang im Körper der Mutter zu behalten, da es sofort nach der Geburt einen Herzschrittmacher benötigt. Je früher das Kind dabei zur Welt kommt, desto schwieriger ist diese Operation und desto höher die Chance, dass etwas schief geht. Ohne die Behandlung ist eine weitergehende Schädigung des Reizleitersystems1 im Herzmuskelbereich wahrscheinlicher, so dass auch dies sich negativ auf die Überlebenschancen auswirkt.
Kurz gesagt: Ohne Behandlung kann die Schädigung fortschreiten, es steigt die Gefahr eines Herzversagens, genauso wie die eines Hydrops oder einer anderen Komplikation.
Mit der Behandlung kommt es zu einer (gesundheitlich wohl neutralen) Veränderung des Gehirngewebes aber die Überlebenschancen steigen möglicherweise (strittig).
Nachdem also durch die Behandlung die Gefahr einer weiteren Herzschädigung deutlich verringert wird, ist es notwendig, dass der Herzschlag des Kindes über 60 Schläge pro Minute (SpM) bleibt. Warum?
Unter 60 SpM steigt die Wahrscheinlichkeit eines Hydrops oder einer anderen Komplikation überproportional an. Daher kann bei einem Wert über 60 eine ambulante Überwachung ausreichend sein, bei einer zweimal wöchentlich stattfindenden Kontrolle per Doppler-Ultraschall. Einmal wöchentlich wird dabei sicherlich im Herzzentrum kontrolliert, das zweite Mal kann aber am Wohnort stattfinden, bzw. in der nächstgelegenen Praxis die ein solches Gerät für Doppler-Ultraschall hat. Falls dies nicht die behandelnde Gynäkologin ist, wird diese die Mutter sicher auch alle ein bis zwei Wochen sehen wollen.
Außerdem steigt bei einem so niedrigen Herzschlag die Gefahr anderer organischer Unterversorgung (bspw. auch des Gehirns). Ab etwa 60 Schlägen kann die Entwicklung ganz normal verlaufen.
Andererseits wird im Rahmen der Behandlungsempfehlung bei einem Abfall des kindlichen Herzschlages unter 60 SpM die Mutter stationär in der Klinik aufgenommen um einerseite medikamentös den Herzschlag von Mutter und Kind (um ca. 5-10 Schläge) zu erhöhen und andererseits eine höhere Kontrolldichte sicherzustellen. Sobald sich nun ein Perikarderguss, ein Hydrops oder eine Endokardfibroelastose bilden, wird eine Geburt notwendig. Es ist wünschenswert, dass diese möglichst spät erfolgt.
Die Geburt

Vor der 28. Schwangerschaftswoche (SSW) ist die Überlebenschance ausgesprochen gering.
Von der 28. SSW an reduziert sich das Risiko nahezu täglich, dies hängt mit der kindlichen Entwicklung im Bauch der Mutter zusammen.
Ab der 34. SSW sind die Chancen gut, denn die Lungenentwicklung ist abgeschlossen. Da das Kind im dritten Trimester aber ca. 200-300 Gramm die Woche zunimmt und wächst, ist es natürlich optimal, wenn die Geburt möglichst nahe dem geplanten Geburtstermin erfolgen kann. Laut unserem Kinderkardiologen “nach der 37. SSW”.
Die Geburt erfolgt per Kaiserschnitt. Ja, ich weiss, das hatte ich noch nicht erwähnt. Es macht aber Sinn, da das geschwächte Kind nicht noch durch den Stress einer normalen Geburt soll. Außerdem muss ja ggf. sofort nach der Geburt der Herzschrittmacher eingesetzt werden. Auch das verständlich kein angenehmer Gedanke aber eine Notwendigkeit.
Ist der Herzschlag deutlich über 60 SpM, kann zwischen der (für das Kind so oder so anstrengenden) Geburt und der Herzschrittmacherimplantation etwas gewartet werden, dies gibt den Kinderkardiologen auch die Gelegenheit, die “Eigenleistung” des Kindes einzuschätzen und zu erkennen und das Kind auch sonst auf mögliche, weitere Schädigungen zu untersuchen.
Die zwei Wochen nach der Geburt sind wohl kritisch, wobei die Überlebenschance proportional zum Alter des Kindes steht.
Wenn aber auch nun alles gut geht, kann Ihr Kind mit Herzschrittmacher, sonst aber weitestgehend normal aufwachsen. Ggf. können Sie sich mit einer örtlichen Selbsthilfegruppe in Verbindung setzen.
Häufige Fragen
… und Korrekturen.
Die Antworten beruhen auf unserem Verständnis aus Gesprächen mit den Ärzten im Pränatalzentrum an der Medizinischen Hochschule Hannover. Generell sollten sie diese Fragen mit dem Arzt Ihres Vertrauens erörtern und dabei ggf. auch die Ärzte des den Fall behandelnden Kinder-Herzzentrums zu Rate ziehen!
Abtreibung
Sicherlich ist dies eine individuelle Entscheidung, wir sind generell aber dagegen, insbesondere wenn es keine sonstigen Gründe gibt. Heutzutage ist das Leben mit einem Herzschrittmacher nahezu uneingeschränkt. Viel zu häufig wird auch bei anderen Herzfehlern abgetrieben, obwohl eine einzige postnatale (nachgeburtliche) Operation den “Fehler” sicher beheben könnte. Selbst wenn dies nicht der Fall ist, wie hier, sollte man dem Kind die Chance geben. Im Falle des AV-Block °III in Verbindung mit dem Sjögren-Syndrom besteht auch ein erhöhtes Risiko für weitere Schwangerschaften, siehe übernächste Frage.
Letztlich können dies nur die Eltern, letztlich nur die Mutter entscheiden. Sie sollten aber vor einer solchen Entscheidung unbedingt das Gespräch mit einem Kinder-Herzzentrum suchen und sich ausführlich beraten lassen!
Belastbare Studien
Unter weitere Lektüre werden diverse Studien genannt. Wie uns dies vermittelt wurde, redet man von einer belastbaren Studie bei mehreren tausend Patienten. Als “grosse Studie” wurde uns die der AEPC über 175 Fälle genannt: Eliason H et al. Circulation 2011; 124:1919-26, die wir aber leider nicht online finden und hier referenzieren konnten. Dies ist jedoch weit von “großen Studien” entfernt und der uns behandelnde Professor wollte sich hier nicht auf “belastbar” festlegen, bezeichnete dies als “hohe Wahrscheinlichkeit”.
In-Uterus Herzschrittmacher-Implantation
Es gibt Kliniken, die dem Kind in der Gebährmutter einen Herzschrittmacher einsetzen. Dies sollte ausschließlich im größten Notfall erfolgen. Ist das Kind bereits so groß, dass es einen Herzschrittmacher eingesetzt bekommen kann, ist die Behandlung eines Frühchens deutlich risikoärmer. Daher ist dies wirklich nur in extremen Ausnahmefällen sinnvoll. Hier empfehlen wir ggf. eine zweite medizinische Meinung einzuholen.
Ich hatte das Sjögren Syndrom, kann ich überhaupt ein Baby bekommen?
Die andere Fragestellung hierzu war, ob eine weitere Schwangerschaft bspw. nach einer Schwangerschaft mit AV-Block überhaupt möglich ist.
Auch wenn Sie das Sjögren Syndrom hatten ist eine Schwangerschaft möglich. Aber!
Es besteht das Risiko einer weiteren Schädigung des ungeborenen Kindes, wie oben beschrieben. Um dieses Risiko weitestgehend zu reduzieren ist eine Kortisonbehandlung vor der Schwangerschaft beginnend und über die komplette Schwangerschaft notwendig. Bei einer Kortisonbehandlung über sechs Monate hinaus sind Nebenwirkungen aber nicht mehr zu 100% reversibel (dass diese wieder vollständig verschwinden), das betrifft Mutter und Kind! Zudem sollte natürlich der behandelnde Gynäkologe informiert sein und entsprechend ggf. eine dichte Kontrolle des Kindes durch Doppler-Ultraschall sicherstellen.
Führen Sie diese Kortisonbehandlung nicht durch, ist mit sehr hoher Wahrscheinlichkeit mit einem pränatalen AV-Block 3. Grades (vollständige, irreparable Zerstörung des Reizleiters1) zu rechnen.
Mit der Behandlung haben Sie eine gute Chance auf ein gesundes Kind (aber keine Sicherheit, die es aber nie gibt).
Kritische Grenze 50 oder 60 SpM?
Es gibt offenbar unterschiedliche Ansichten, wo die “kritische Grenze” liegt. Häufig in der medizinischen Literatur wird diese Grenze bei 50 SpM (HerzSchläge pro Minute) definiert. Die Medizinische Hochschule Hannover (Prof. Dr. von Kaisenberg) definierte sie uns gegenüber bei 60 SpM. Ich erlaube mir da die folgende Interpretation. Kritisch-kritisch sind wohl 50 SpM, aber bereits bei 60 SpM kann es kritisch werden und eine erhöhte Kontrolldichte (Einweisung ins Pränatalzentrum) ist wohl angebracht.
Reizleiter oder Nerv?
Der Mediziner spricht korrekterweise vom “Reizleitersystem, welches für den Herzschlag verantwortlich ist. Dies sind keine “Nerven”, sondern modifizierte Muskelfasern, wenn sie auch für Laien die gleiche Aufgabe übernehmen, sie stimulieren das Herz zum Schlagen. Sie sind aber anders aufgebaut, weshalb hier die Antikörper angreifen und normale Nervenzellen und -bahnen nicht betroffen sind. Ob die Antikörper ggf. andere Muskeln im Aufbau ebenfalls zerstören können ist mir noch nicht klar.
Weitere Lektüre
Wir selbst haben ja in unserer Zusammenfassung auf eine deutsche Studie Bezug genommen, deren Informationen zum pränatalen AV-Block °III wir hier zusammengefasst haben. Ursprünglich erhielten wir von den Experten der Medizinischen Hochschule Hannover eine Referenz auf eine kanadische Studie, The Benefits of Transplacental Treatment of Isolated Congenital Complete Heart Block Associated with Maternal Anti-Ro ⁄ SSA Antibodies: A Review, die im verlinkten Online Library von Wiley.com eingesehen werden kann.
Sollten Sie weitere Informationen kennen, bitte ich Sie freundlich um entsprechende Information!
Wikipedia-Diskrepanzen
In Wikipedia gibt es in der entsprechenden Seite kurze Informationen zu pränatalem AV-Block. Wikipedia refernziert hier eine Veröffentlichung zu Herzschrittmacher- und Defibrillatortherapie aus der wir eine Abschrift der Passagen erstellt haben, die sich mit dem angeborenen (nicht pränatalen) AV-Block III. Grades befassen und die für uns eine große Hilfe waren, die Fakten in einen logischen Zusammenhang zu bringen. Aus dieser Veröffentlichung bleiben dennoch viele Fragen offen, auf die ich (gern mit Hilfe) versuchen werde, Antworten zu finden und hier zusammen zu fassen.
Fehler, Ergänzungen
Die Informationen auf dieser Website wurden nach bestem Wissen und Gewissen zusammengestellt. Diese Seite nimmt keine Vollständigkeit für sich in Anspruch und auch sind andere Behandlungsmethoden denkbar. Wenn Sie der Meinung sind, dass hier ergänzende Informationen oder auch Meinungen notwendig sind oder wenn sie richtige Fehler finden, kontaktieren Sie mich bitte oder hinterlassen Sie einen Kommentar.
Anmerkung; Ich habe irgendwo “Typ 3” aufgeschnappt. Ich wurde nachdrücklich darauf hingewiesen, dass dies medizinisch nicht korrekt sei. Ich habe es aber auch bei Suche im Internet gefunden, weshalb ich die Bezeichnung in den Suchbegriffen in den Metadaten behalten habe.
The Quick Summary
If you diagnosed or got diagnosed a prenatal, connatal or congenital AV-Block °III, an atrioventricular block, 3. grade or a congenital complete heart block without anything else out of the ordinary, you should immediately order a blood test of the mother to check Ro and La AK! In addition, Anti Phospholipid AK should be checked (Anti Cardiolipin).
If the heartbeat is below 60 bpm (beats per minute), you should also check for a pericardial_effusion, hydrops and (rare) endocardial fibroelastosis. With a positive medical evidence, or should there be anything else out of the ordinary the attending physician shall contact immediately the closest prenatal center with experience of heart disorders (Prenatal Cardiac Center). Depending on the exact diagnosis, an emergency referral to that Prenatal Cardiac Center (by ambulance if necessary) is likely! The child is in mortal danger, (further) fetal damage to organs or prenatal development can not be ruled out.
If the heartbeat is below 60 bpm but there is no other disorder, complication or other unusual diagnosis, the next Prenatal Cardiac Center should also be contacted immediately. An immediate referral into hospital is also necessary, though in this case, the attending physician may be instructed to medically stimulate the heartbeat before (by 5-10 bpm).
If the heartbeat remains above 60 bpm with none of the above mentioned complications, the chances are quite good to stop the negative development and, aside of a necessary pacemaker, the child may be completely healthy. No, it is not sure! Doctor or mother should also contact the next Prenatal Cardiac Center and request an appointment at earliest convenience! Earliest convenience means, the appointment does not have to be the same day! It is imperative to involve a Prenatal Cardiac Center, not every Prenatal Center and not every doctor appreciates sufficient experience!
More information about the further treatment follows. But first the diagnosis…
What is a prenatal AV-Block Type 3?
First of all, it is diagnosed (named) differently, sometimes as prenatal (pre-birth), sometimes congenital or connatal (both meaning “inborn”). Sometimes as an AV-Block 3rd Grade, sometimes associated with a bradycardia (slow heartbeat), sometimes as a complete or an atrioventricular block, sometimes simplified as a complete heart block or abbreviated as AVB or AVB3.
Whoever hears that diagnosis the first time, does not know anything about it and finds a lot of misleading or incorrect information on the web, most of it arousing panic. As we learned, many doctors have the same reaction, the diagnosis being so very very rare – only one out of 20,000 live births! With more than 660,000 births in Germany 2012 that would be 33 births/year in Germany, in Hanover at the medical university there are about 1-2 cases a year. With about 4 Mio. births in the U.S., it is just about 200 cases a year there.
Without wanting to belittle the diagnosis: If you are confronted with it, something very bad happened: Likely the CCS, the Cardiac Conduction System (CCS)1, responsible for the heart beat got irreparably damaged.
As bad as that diagnosis is and sounds, everything else can be managed! And if everything works out find, your child “just” gets a pacemaker, but in reality, that poses only little restrictions! Please keep reading!!
![]() The following information is not scientifically founded yet but are based on medical experiences, assessments and recommendations. As of the low number of cases, to our knowledge there are no reliable2 studies or results!
The following information is not scientifically founded yet but are based on medical experiences, assessments and recommendations. As of the low number of cases, to our knowledge there are no reliable2 studies or results!
There are though studies with limited numbers of patients they are based on, which findings have lead to recommendations on how to handle the diagnosis, which is the base of what we write here. Some of the studies are found at the end of the page under Further Reading.
The likely reasons for a prenatal AV-Block Type 3
The diagnosis of a (complete) prenatal AV-Block Type 3 comes in three different manifestations, representing roughly about one third of the cases.
Variant 1 is in combination with a so-called congenital heart disorder, a born-in one, whereas in these cases, the entire heart and the organic development are also affected.
Variant 2 is called idiopathic, meaning there is no comprehensible reason.
Variant 3 is related to an auto-immune reaction with the mother. It is not a disorder, as an anti-immune reaction usually is “healthy”. Do they though turn against healthy body tissue they cause sickness and it’s called an anti-immune disorder.
To my knowledge, this is generally the only confirmed cause, so this is what we can try to explain here.
AV-Block Type 3 + Sjörgren Syndrome
The cause for this AV-Block is likely a rheumatic reaction, a so-called Sjögren Syndrome of the mother, which can have happened long before the pregnancy. Very often, this disorder is not even noticed! As a result of this rheumatic reaction, the body has developed anti-bodies, so-called Ro and La AK, which then keep residing in the mother’s body.
These antibodies have been created by immune defense to counter a disease/disorder in the mother and as such are not generally hostile.
But now comes the pregnancy. Between pregnancy week 18 and 20, the antibodies, including these Ro and La AK penetrate through the placenta into the child’s body. In general a good idea, such giving the child the immunisation of the mother. In the case of Ro and La AK now there is a malfunction. These antibopdies “understand” the developing nerves at the child’s heart as rheumatic. In countering the (nonexisting) “rheumatic disorder” they unintentionally distroy the cardiac conduction system1! This happens first at the connection from the heart’s nerve node, the so-called AV-node to the hearts main chambers, which is why the diagnosis got this name. There are different manifestations, from a partial disorder to the complete destruction, being also named 3rd grade then (also written °III).
In many cases, this is fatal for the child. But then you would likely not read this. In other cases, the heart remains beating, thanks to secondary stimuli and nerves, but distinctly slowed. If there is a correlation between the mother’s heartbeat and that remaining one of the child, I have contradictory information about.
In the case I know (our own), the heartbeat collapsed to 62-63 beats per minute (bpm). Normal would be 110-160 bpm.
I have been asked to also mention the more rare case of a systemic lupus erythematosus (also called lupus or SLE). Sjögren Syndrome and SLE are two manifestations of a rheumatic anti-immune disorder with different symptoms, both should be identified by testing for Ro and LaAK antibodies.
The Diagnosis. What now?
 Imperative: Speed! As the antibodies are still active in the fetus, further damage is possible, more even likely. As such, quick response to the threat is important. Not to improve the situation but to avoid further damage and harm.
Imperative: Speed! As the antibodies are still active in the fetus, further damage is possible, more even likely. As such, quick response to the threat is important. Not to improve the situation but to avoid further damage and harm.
The diagnosis itself does not say anything, especially not about the further chances for survival of the child. Furthermore, this diagnosis is not sign for a mental “handicap” of the child whatsover!
Important is first and foremost to rule out further complications and such further damage.
Common complications are the above mentioned pericardial_effusion, hydrops and endocardial fibroelastosis (the links open a new window). Whereas a small pericardial effusion is relatively “normal” and may be simply monitored. But specialized physicians of Prenatal Cardiac Centers can better evaluate that!
To avoid further damage of the fetus development of the cardiac conduction system1 is kind of difficult. As the diagnosis is so rare, there are no reliable studies2. But on earlier studies there, at the Hospital for Sick Children in Toronto (Canada) follows the therapeutic policy to apply mothers with a diagnosed fetal complete heart block with a frequency below 55 bpm (beats per minute) Dexamethason and a Betamimetica (to stimulate the β-receptors, the oppositve of β-blockers). This is opposed by the major AEPC-study, which did not find any improvement to the fetal survival rate for children treated with Cortisone. This study considers the time of diagnosis below 20 weeks, a heart frequency under 50 bpm, a hydrops and a reduced LV-funtion as especially unfavorable for the prognosis. On the other side, other authors (as also Prof. Dr. von Kaisenberg at the Hanover Medical University) recommend the therapy with steroids to avoid the hydrops.
(As any other treatment) Such a steroid-therapy has also its side-effects. Most notably is a change of the organic tissue in the fetal brain. But there is no medical evidence of any other negative side effects caused by that change in the organic tissue. But there is also no conclusive information that rules out such negative side-effects.
As the experimental treatments have shown so far is that it largely reduces the danger of further damage, the survival factor of the children increased from 80% before testing the treatment to 95% after. And before, the survival chance of the child for the first year (weeks) after the birth (postnatal) was only 47%. Though without having hard facts, the following interpretation can be considered as likely:
“Despite missing prospective studies, fluoride corticoids are recommended for fetuses with incomplete AV-Block and Hydrops. If the AV-Block is completely established, regression has not, but advancing of the blockade from a second- to third-grade block have been reported.” (German Source). But also with a third-grade AV-Block there is an imminent danger of further damage by the antibodies! Therefore such therapy seems recommendable until the end of the pregnancy!
The treatment is about keeping the child as long as possible in the mother’s womb, as it will need a pacemaker right after birth. The earlier the child is delivered, the more difficult that operation and the more likely the chance something goes wrong. Without the treatment, a further damage of the tissue in the CCS1 is possible, having a negative impact on the survival chances again.
In short: Without treatment the damage can get worse, the danger of a heart failure increases, as well as of a hydrops or other complications. With the treatment, there will be a (medically possibly neutral) alteration of the brain tissue, but the survival chances increase (disputed).
Having the danger of further damaged reduced, it remains important to keep the baby’s heart beat above 60 beats per minute (bpm). Why?
Under 60 bpm, the chances for a hydrops or other complications increase exponentially. Therefore a value above 60 can justify an ambulatory treatment with a twice-weekly check by Doppler ultrasonic. One a week in the Prenatal Cardiac Center, once a week can be at your hometown, respectively the next doctor’s office having such a device. If that is not the treating gynecologist, the mother will likely want to see the own gynecologists bi-weekly.
In addition, with such a low heartbeat the danger of organic nourishment shortages (incl. the brain) increases. Above 60 bpm the development can proceed quite normal.
On the other side, as part of the suggested treatment, when the fetal heartbeat drops below 60 bpm, the mother should be hospitalized to receive a medical treatment to increase the heartbeat of mother and child (by about 5-10 bpm) and increase the monitoring checks. Should now a pericardial effusion, hydrops and endocardial fibroelastosis develop, delivery (birth) becomes a necessity. The goal is to have this happen as late as possible.
The Birth

Before pregnancy week 28 the survival chances are considerably low.
From the 28th pregnancy week onward, the risk reduces at a daily rate, being a result of the fetal development in the womb.
From the 34th week the chances are good, the lung development has been finished. But as the child gains about 200-300 grams a week (7-10 oz) and grows, it sure is best if the birth can happen as close to the planned birth date as possible. According to our Prenatal Cardiac Doctor “after the 37th week”.
Delivery is done by C-section. Yes, I know, I did not mention that yet. But it makes sense, not to stress the weakened fetus further by the stresses of a normal birth. And right after birth the pacemaker shall be implanted. This too sure not being a happy thought, but a necessity.
If the heartbeat remains notably above 60 bpm the implantation of the pacemaker can be deferred to allow the child to recover from the birth stress. This also allows the child cardiologists to monitor and understand the child’s own capacity and check the child for further possible damage.
The two weeks following the birth and pacemaker implementation are critical, whereas the chance for survival is proportional to the “age” of the child.
If now everything turns out well, your child can grow up with a pacemaker, but otherwise mostly normal. If you feel so, you can contact one of the local self-help-groups.
Frequently Asked Questions
… and corrections
The answers reflect our understanding from discussions and talks with the physicians and doctors at the Hanover Medical University. In General, you should address these questions with the physician of your choice and possibly involve the doctors of the Prenatal Cardiac Center managing that individual case!
Abortion
Sure, it is a personal decision. But we oppose it usually, especially if there are no other sound reasons. Today, life with a pacemaker is almost uninhibited. Far too often these and other children with heart disfunctions or problems are being aborted, even where a single, postnatal operation could safely correct the “problem” permanently. Even where this is not the case, like here, you should give the child a chance. In the case of an AV-Block with Sjörgen-Syndrome you also have an increased risk for further pregnancy, seen question after next.
In the end, only the parents, ultimately only the mother can decide. But in any case, before such a decision you should definitely consult about this with the experts at your next Prenatal Cardiac Center and get a proper and complete briefing.
Cardiac Conduction System, are that nerves?
The physician correctly calls it Cardiac Conduction System (or CCS), being responsible for the heart beat. This are not “nerves” but modified muscle fiber, though they do have the same task for the amateur; they stimulate the heart to beat. They are differently constructed, which is why the antibodies attack here, but not the nerve cells and fibers. If the antibodies attack other muscles is not yet clear to me.
Critical Heartbeat 50 or 60 bpm
There are different opinions obviously about when the heartbeat becomes “critical”. In most medical literature, 50 bpm (beats per minute) is considered “critical”. At the Medial University of Hanover, Prof. Dr. von Kaisenberg specified “critical” as 60 bpm. So I allow myself the following interpretation. Critical-critical is 50 bpm, but from 60 bpm we come into a critical range that may make an increased monitoring (hospitalization) recommendable.
Further Reading
Our Prenatal Cardiac Center at the Medical University of Hanover has referred us initially to a Canadian Study: The Benefits of Transplacental Treatment of Isolated Congenital Complete Heart Block Associated with Maternal Anti-Ro ⁄ SSA Antibodies: A Review, published (as linked) in the Wiley Online Library.
For the page, we also used a German study, of which we extracted the paragraphs related to our topic here.
If you learn about other publications you believe noteworthy, please let us know!
In-Uterus heart pacemaker implantation
There are clinics implanting the pacemaker in uterus (in the womb). This should be the absolute exception for severe emergencies. If the child is grown enough to get a pacemaker, the managing of an early-born is usually far less risky. So this is really only reasonable in very extreme exceptions. We urge you to get a second medical assessment from a different clinic.
I had the Sjörgren Syndrome, can I get a baby at all?
The different question was if another pregnancy would be possible at all after a pregnancy that came up with an AV-Block.
Even if you had the Sjörgen Syndrome, another pregnancy is possible. But!
There is the risk of a nerv damaging for the unborn child as explained above. To minimize that risk best possible, a cortisone treatment shall begin before the pregnancy already and must be maintained on throughout the complete pregnancy. With a Cortisone treatment for more than six months the side effects are usually no longer completely reversible (that they cease completely), that refers to mother and child! The gynecologist should sure be completely informed and make sure of a frequent check with Doppler-ultrasonic.
If you do not do that Cortisone treatment, you have a very high likeliness of an AV-block °III (complete, irreversible damage of the nerves).
With the treatment, you have a good chance for a healthy child (though no safety, but that’s non-existing anyway).
Studies – why do you call them unreliable?
We refer to several studies in Further Reading. As we were made to understand, you call a study “reliable” when several thousand patients took part. As a “major study” the AEPC was named with 175 cases: Eliason H et al. Circulation 2011; 124:1919-26 which we did not find online to link here. This is far from any “major study” and our attending professor did not want to use “reliable”, instead calling it “highly probable”.
Wikipedia-Discrepancies
In Wikipedia there are some pages with short information about the prenatal (congenital) AV-block. The short publication leaves more questions than it provides answers, but I will try (happily with your help) to collect and consolidate answers to be publish here (and maybe also extend Wikipedia).
Errors, Amendments
The information on this website has been compiled best to individual knowledge and understanding. The page does not imply to be complete or to contain all the information available. Other possibilities to treat this diagnosis are conceivable. Should you believe the page to show additional information or opinions or if you find real errors, please contact me or leave a comment!
Remark: I have somewhere taken up “Type 3”. It was emphasized to me that this is medically incorrect. Having found that definition also on the Internet, I kept the keyword in the Meta-tags of this page.